 |
The literature is full of references that
victims are reluctant to disclose IPV/DV to healthcare providers
and that healthcare providers are reluctant to ask patients
about IPV/DV. Most commonly cited reasons that patients do
not disclose is:
- Fear of retaliation by the abuser;
- Shame, humiliation and denial about the seriousness of
the abuse; and
- Concern about confidentiality, especially related to law
enforcement involvement.
In cases when injuries and health problems are apparent
and well documented, healthcare providers often do not ask
about IPV/DV or intervene on behalf of their patients who
experience it. One study found that only 6 percent of physicians
ask their patients about possible IPV/DV, yet 88 percent admitted
that they knew they had female patients who had been abused.
Another study indicated that 48 percent of women supported
routine screening of all women, with 86 percent stating it
would make it easier to get help (Kass-Bartlesme, 2004).
Healthcare providers have said that they do not screen for
IPV/DV because (Darrow, et al, 2007; Tjaden, P. & Thoennes,
N., 2002; Borowsky, I.W., Ireland, M., 2002; Elliott, L.,
Nerney, M., Jones, T., et al., 2002; Gerbert, et. al., 1999):
- They lack the necessary training and education, time,
tools, and support resources, and
- Fear of offending the patient;
- Frustration with the lack of change in the patient's situation
or frustrations with the patient's unresponsiveness to advice;
- They do not feel they can make a difference;
- Feelings of powerlessness to "fix" the situation; and
- Their sense of loss of control over the patient's decision
making.
An AHRQ-funded survey found that many primary care clinicians,
nurses, physician assistants, and medical assistants lack
confidence in their ability to manage and care for victims
of IPV/DV (Sugg, et. al., 1999):
- Only 22 percent had attended any educational program on
IPV/DV within the previous year;
- Over 25 percent of physicians and nearly 50 percent of
nurses, physician assistants, and medical assistants stated
that they were not at all confident in asking their patients
about physical abuse;
- Less than 20 percent of clinicians asked about IPV/DV
when treating their patients for high-risk conditions such
as injuries, depression or anxiety, chronic pelvic pain,
headache, and irritable bowel syndrome;
- Only 23 percent of physicians, nurses, physician assistants,
and medical assistants believed they had strategies that
could assist victims of IPV/DV.
A recent study of emergency department nurses (Darrow, et
al., 2007) identified the following barriers to screening
patients for IPV/DV:
- Language difference;
- Lack of training in how to deal with abuse; and
- Time issues affected their ability to adequately screen
patients.
For information regarding the specific studies referred to
above, go to http://www.ahrq.gov/research/domviolria/domviolria.htm#more.
Darrow, et al., (2007) also identified personal or family
history of abuse as a factor why nurses do not screen for
IPV/DV.
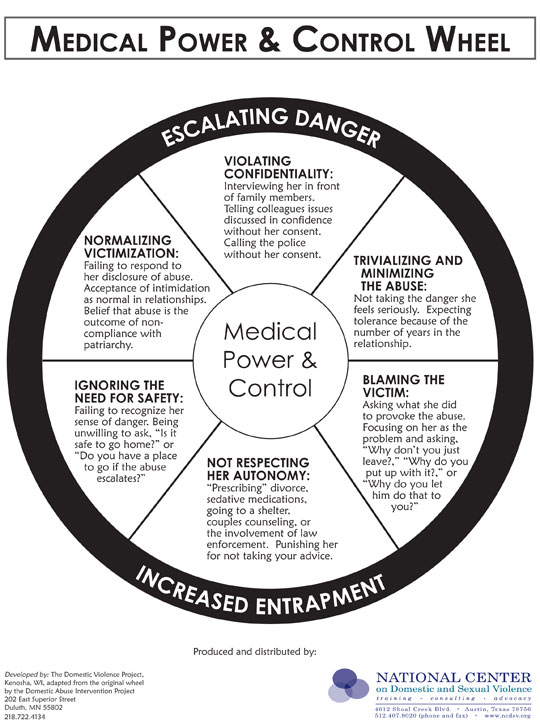
Medical Power and Control Wheel
Just as with the previously identified Power and Control
Wheel identifying the dynamics of abuse in the IPV/DV, the
Medical Power and Control Wheel identifies how healthcare
providers contribute to the problems of IPV/DV for the victim.
These include violating confidentiality; trivializing, minimizing
or normalizing the abuse, blaming the victim, taking a patriarchal
tone by telling the victim what she should do and not taking
the victims safety needs seriously.
Continue on to Best
Practice Guidelines
|
 |