 |
 Bacillus anthracis
Bacillus anthracis The "Chain of Infection" is a basic component
of understanding the prevention and control of infection that
most healthcare workers recall from their early days of training.
It is a critical concept in infection control that is worth
reviewing:
Chain of Infection
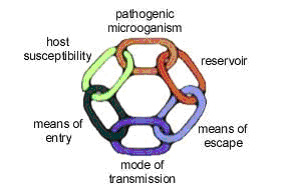
The pathogen is the microorganism that
causes infection. They include bacteria, viruses, fungi and
parasites. There must be an adequate number of pathogens to
cause disease. Infectious agents transmitted during healthcare
derive primarily from human sources but inanimate environmental
sources have also been implicated in transmission (Siegel,
et al., 2007).
The reservoir is the place where microorganisms
live, such as in humans and animals, in soils, food, plants,
air or water. The reservoir must meet the needs of the pathogen
in order for the pathogen to survive and multiply. Human reservoirs
include patients, healthcare personnel, and household members
and other visitors. Such source individuals may have active
infections, may be in the asymptomatic and/or incubation period
of an infectious disease, or may be transiently or chronically
colonized with pathogenic microorganisms, particularly in
the respiratory and gastrointestinal tracts. The endogenous
flora of patients (e.g., bacteria residing in the respiratory
or gastrointestinal tract) also are the source of HAIs (Siegel,
et al., 2007).
The means of escape are how the microorganism leaves
the reservoir. These portals can be:
- Respiratory- for example, viruses that cause the common
cold, Mycobacterium. tuberculosis, and Haemophilus influenza
utilizes this means of exit from the reservoir.
- Genitourinary- for example, sexually transmitted diseases
such as syphillus or HIV.
- Alimentary - for example, salmonella, rotavirus, C. difficile,
Giardia.
- Skin - for example, scabies, impetigo.
- Blood and body fluids - HIV, Hepatitis B and C.
- Transplancental - for example, Rubella and HIV.
Some microorganisms have more than one means of escape -
for example, chickenpox can be spread via respiratory source
or the patient's skin. Bloodborne pathogens such as HIV, Hepatitis
B and C can be spread through blood and from fluid from the
genitourinary system.
The mode of transmission is how the pathogen
moves from place to place. This can occur through three principle
routes:
- Contact transmission, which is further divided
into (Siegel, et al., 2007):
- Direct transmission occurs when microorganisms
are transferred from one infected person to another
person without a contaminated intermediate object or
person. Opportunities for direct contact transmission
between patients and healthcare personnel include:
- blood or other blood-containing body fluids from
a patient directlyenters a caregiver's body through
contact with a mucous membrane or breaks (i.e.,
cuts, abrasions) in the skin.
- mites from a scabies-infested patient are transferred
to the skin of a caregiver while he/she is having
direct ungloved contact with the patient's skin.
- a healthcare provider develops herpetic whitlow
on a finger after contact with HSV when providing
oral care to a patient without using gloves or HSV
is transmitted to a patient from a herpetic whitlow
on an ungloved hand of a healthcare worker.
- Indirect transmission involves the transfer
of an infectious agent through a contaminated intermediate
object or person. In the absence of a point-source outbreak,
it is difficult to determine how indirect transmission
occurs. However, extensive evidence suggests that the
contaminated hands of healthcare personnel are important
contributors to indirect contact transmission. Examples
of opportunities for indirect contact transmission include
(Siegel, et al., 2007):
- Hands of healthcare personnel may transmit pathogens
after touching an infected or colonized body site
on one patient or a contaminated inanimate object,
if hand hygiene is not performed before touching
another patient.
- Patient-care devices (e.g., electronic thermometers,
glucose monitoring devices) may transmit pathogens
if devices contaminated with blood or body fluids
are shared between patients without cleaning and
disinfecting between patients.
- Shared toys may become a vehicle for transmitting
respiratory viruses or pathogenic bacteria among
pediatric patients.
- Instruments that are inadequately cleaned between
patients before disinfection or sterilization (e.g.,
endoscopes or surgical instruments) or that have
manufacturing defects that interfere with the effectiveness
of reprocessing may transmit bacterial and viral
pathogens.
- Clothing, uniforms, laboratory coats, or isolation
gowns used as personal protective equipment (PPE),
may become contaminated with potential pathogens
after care of a patient colonized or infected with
an infectious agent. Although contaminated clothing
has not been implicated directly in transmission,
the potential exists for soiled garments to transfer
infectious agents to successive patients.
- Droplet transmission is, technically, a form of
contact transmission, and some infectious agents transmitted
by the droplet route also may be transmitted by the direct
and indirect contact routes. However, in contrast to contact
transmission, respiratory droplets carrying infectious pathogens
transmit infection when they travel directly from the respiratory
tract of the infectious individual to susceptible mucosal
surfaces of the recipient, generally over short distances,
necessitating facial protection. Respiratory droplets are
generated when an infected person coughs, sneezes, or talks
or during procedures such as suctioning, endotracheal intubation,
cough induction by chest physiotherapy and cardiopulmonary
resuscitation (Siegel, et al., 2007).
Studies have shown that the nasal mucosa, conjunctivae
and less frequently the mouth, are susceptible portals
of entry for respiratory viruses. The maximum distance
for droplet transmission is currently unresolved; historically,
the area of defined risk has been a distance of less than
3 feet around the patient. Using this distance for donning
masks has been effective in preventing transmission of
infectious agents via the droplet route. There is some
evidence to suggest that some droplets (SARS and smallpox)
could reach persons located 6 feet or more from their
source. It is likely that the distance droplets travel
depends on the velocity and mechanism by which respiratory
droplets are propelled from the source, the density of
respiratory secretions, environmental factors such as
temperature and humidity, and the ability of the pathogen
to maintain infectivity over that distance. Based on these
considerations, it may be prudent to don a mask when within
6 to 10 feet of the patient or upon entry into the patient's
room, especially when exposure to emerging or highly virulent
pathogens is likely. More studies are needed to improve
understanding of droplet transmission under various circumstances
(Siegel, et al., 2007).
Droplet size is another variable under discussion. Droplets
traditionally have been defined as being >5 Ám in size.
Droplet nuclei, particles arising from desiccation of
suspended droplets, have been associated with airborne
transmission and defined as <5 Ám in size. Observations
of particle dynamics have demonstrated that a range of
droplet sizes, including those with diameters of 30 microns
or greater, can remain suspended in the air. The behavior
of droplets and droplet nuclei affect recommendations
for preventing transmission. Whereas fine airborne particles
containing infectious pathogens can remain a lot in the
air, requiring an airborne infection isolation room (AIIR)
to prevent its dissemination within a facility; organisms
transmitted by the droplet route cannot remain aloft in
the air and therefore do not require special air handling
and ventilation. Examples of infectious agents that are
transmitted via the droplet route include Bordetella
pertussis, influenza virus 23, adenovirus 111 , rhinovirus,
Mycoplasma pneumoniae, SARS-associated coronavirus
(SARS-CoV), group A streptococcus, and Neisseria meningitides
(Siegel, et al., 2007)."
- Airborne transmission occurs by dissemination of
either airborne droplet nuclei or small particles in the
respirable size range containing infectious agents that
remain a lot in the air over time and distance (e.g., spores
of Aspergillus spp, and Mycobacterium tuberculosis)
(Siegel, et al., 2007).
Microorganisms carried in this manner may be dispersed
over long distances by air currents and may be inhaled
by susceptible individuals who have not had face-to-face
contact with (or been in the same room with) the infectious
individual. Preventing the spread of pathogens that
are transmitted by the airborne route requires the use
of special air handling and ventilation systems (e.g.,
AIIRs) to contain and then safely remove the infectious
agent. Infectious agents to which this applies include
Mycobacterium tuberculosis, rubeola virus (measles),
and varicella-zoster virus (chickenpox). In addition,
published data suggest the possibility that variola
virus (smallpox) may be transmitted over long distances
through the air under unusual circumstances and AIIRs
are recommended for this agent as well; however, droplet
and contact routes are the more frequent routes of transmission
for smallpox. In addition to AIIRs, respiratory protection
with NIOSH certified N95 or higher level respirator
is recommended for healthcare personnel entering the
AIIR to prevent acquisition of airborne infectious agents
(Siegel, et al., 2007).
The means of entry is how the microorganism enters
the host. Often this is the same means from which the organism
left the reservoir.
The susceptible host is the person who may become
infected. Infection is the result of a complex interrelationship
between a potential host and an infectious agent. Most of
the factors that influence infection and the occurrence and
severity of disease are related to the host. However, characteristics
of the host-agent interaction as it relates to pathogenicity,
virulence and antigenicity are also important, as are the
infectious dose, mechanisms of disease production and route
of exposure. There is a spectrum of possible outcomes following
exposure to an infectious agent.
Some persons exposed to pathogenic microorganisms never develop
symptomatic disease while others become severely ill and even
die (Siegel, et al., 2007). Some individuals are prone to
becoming transiently or permanently colonized but remain asymptomatic.
Still others progress from colonization to symptomatic disease
either immediately following exposure, or after a period of
asymptomatic colonization. The immune state at the time of
exposure to an infectious agent, interaction between pathogens,
and virulence factors intrinsic to the agent are important
predictors of an individuals' outcome (Siegel, et al., 2007).
Host factors such as extremes of age and underlying disease
(e.g. diabetes), human immunodeficiency virus/acquired immune
deficiency syndrome [HIV/AIDS], malignancy, and transplants
can increase susceptibility to infection as do a variety of
medications that alter the normal flora (e.g., antimicrobial
agents, gastric acid suppressants, corticosteroids, antirejection
drugs, antineoplastic agents, and immunosuppressive drugs).
Surgical procedures and radiation therapy impair defenses
of the skin and other involved organ systems. Indwelling devices
such as urinary catheters, endotracheal tubes, central venous
and arterial catheters and synthetic implants facilitate development
of HAIs by allowing potential pathogens to bypass local defenses
that would ordinarily impede their invasion and by providing
surfaces for development of biofilms that may facilitate adherence
of microorganisms and protect from antimicrobial activity.
Some infections associated with invasive procedures result
from transmission within the healthcare facility, others arise
from the patient's endogenous flora.
The host may also have acquired immunity to the pathogen
such as may occur through previous infection with the pathogen
or through immunization (Siegel, et al., 2007).
The occurrence and presence of all these factors and events
is considered the "chain of infection". In the healthcare
setting, all of these factors come into play in the spread
and the control of infection. Effective infection control
strategies prevent disease transmission by interrupting one
or more links in the chain of infection (CDC, 2003).
Continue to: Element II,
Con't.
|
 |