 |
As previously stated, HAIs are a serious problem in healthcare.
Every year an estimated 2 million patients acquire HAIs; 99,000
die from their infection. Many infections are transmitted
on the hands of healthcare providers and personnel. One of
the most important methods for breaking the chain of infection
is hand hygiene and hand washing. Despite the sophistication
healthcare and the science behind that care, the simple and
low-tech intervention of hand hygiene is a significant factor
in reducing the spread of infection.
According to the CDC (2002), healthcare personnel only practice
hand hygiene about half the time. In the CDC Guidelines
for Isolation Precautions: Preventing Transmission of Infectious
Agents in the Healthcare Setting (2007), multiple research
regarding healthcare professionals and hand hygiene were summarized:
Differences in observed adherence to proper handwashing and
hand hygiene were reported among occupational groups in the
same healthcare facility and between experienced and nonexperienced
professionals. The self-reports of healthcare providers indicated
higher adherence than those reported in observational studies.
Among nurses and physicians, the number of years of experience
was a negative predictor of adherence. Education was used
as the primary intervention to improve adherence in most studies.
While positive changes in knowledge and attitude were demonstrated,
accompanying behavioral changes were limited or did not occur.
Use of engineering controls and facility design concepts for
improving adherence is gaining interest.
The hand hygiene guidelines presented here were developed
by the CDC's Healthcare Infection Control Practices Advisory
Committee (HICPAC), in collaboration with the Society for
Healthcare Epidemiology of America (SHEA), the Association
of Professionals in Infection Control and Epidemiology (APIC),
the Infectious Disease Society of America (IDSA) (2003).
Handwashing should occur (CDC, 2002):
- Whenever hands are visibly dirty or contaminated.
- Before:
- having contact with patients
- putting on gloves before inserting any invasive device
- manipulating an invasive device
- After:
- having contact with a patient's skin
- having contact with bodily fluids or excretions,
non-intact skin, wound dressings, contaminated items
- having contact with inanimate objects near a patient
- removing gloves
It is important to remember that even if the healthcare provider
did not touch the patient, bacteria can survive for days on
patient care equipment and other surfaces in the patient care
environment, including bed rails, IV pumps, computer keyboards,
etc. Practicing hand hygiene after leaving the patient's room,
even when the patient was not touched, is imperative to prevent
the transmission of pathogens (CDC, 2003).
Persistence of Bacteria and Viruses on
Dry/Inanimate Surfaces
(Kramer, Schwebke & Kampf, 2006)
Acinetobacter species —› 3 days
- 5 months
C. difficile (spores) —›
5 months
E. coli —› 1.5 hours - 16 months
Enterococci —› 5 days - 4 months
Klebsiella species —› 2 hours to
>30 months
Pseudomonas —› 6 hours - 16 months
Staphylococcus aureus —›
7 days - 7 months
Influenza —› 1-2 days
Rotavirus —› 6 -60 days
Alcohol-based hand rubs, either foam or gel, kill more effectively
and more quickly than handwashing with soap and water. They
are also less damaging to the skin, resulting in less dryness
and irritation, leading to fewer breaks in the skin. Hand
rubs require less time than handwashing with soap and water
and bottles/dispensers can be conveniently placed at the point
of care, to be more accessible (CDC, 2003).
ALCOHOL-BASED HAND
RUBS ARE MORE EFFECTIVE IN KILLING BACTERIA THAN SOAP AND
WATER
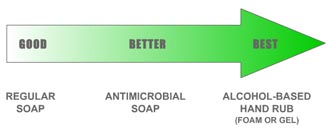
An alcohol-based hand rub is the preferred method
for hand hygiene in all situations, except for when your hands
are visibly dirty or contaminated.
HAND RUB (foam and gel)
- Apply to palm of one hand (the amount used depends on
specific hand rub product).
- Rub hands together, covering all surfaces, focusing in
particular on the fingertips and fingernails, until dry.
Use enough rub to require at least 15 seconds to dry.
HANDWASHING
- Wet hands with water.
- Apply soap.
- Rub hands together for at least 15 seconds, covering
all surfaces, focusing on fingertips and fingernails.
- Rinse under running water and dry with disposable towel.
- Use the towel to turn off the faucet.
|
Colleagues, trainees, and other staff watch one another
(CDC, 2003):
- Research has shown that the actions of clinicians
influence the behavior of others.
- Show your colleagues that hand hygiene is an
important part of quality care. Patients also watch
what healthcare providers do:
- As a healthcare provider, your actions send
a powerful message.
- Show your patients that you are serious about
their health.
|
Hand lotions are important to prevent skin dryness and irritation.
You should use only hospital-approved hand lotions. Other
lotions may (CDC, 2002):
- Make hand hygiene less effective.
- Cause breakdown of latex gloves.
- Become contaminated with bacteria if dispensers are refilled.
Artificial Nails (CDC, 2002):
- Healthcare workers who have direct contact with high-risk
patients (e.g., ICU, OR) should not wear artificial nails,
tips, wraps, etc.
- Natural fingernails should be kept to a length of approximately
¼ inch past the tip of the finger.
- Nail polish is acceptable, but should not be chipped.
Continue to Element
III
|
 |