 |
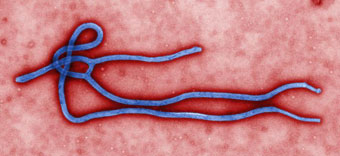 This colorized transmission electron micrograph
(TEM) revealed some of the ultrastructural morphology displayed
by an Ebola virus virion. Photo courtesy of CDC/Cynthia
Goldsmith.
This colorized transmission electron micrograph
(TEM) revealed some of the ultrastructural morphology displayed
by an Ebola virus virion. Photo courtesy of CDC/Cynthia
Goldsmith. Because of their contact with
patients or infective material from patients, environmental
services and facility visitors, healthcare workers and healthcare
organizations utilize multiple interventions to prevent and/or
manage infections in healthcare workers.
Initially, new employees are
generally required to have a pre-employment physical; presumably
any infection can be identified at that time and treatment
initiated or management strategies employed prior to contact
with patients or coworkers. Because healthcare workers are
at risk for exposure to and possible transmission of vaccine-preventable
diseases, maintenance of immunity is an essential part of
prevention and infection control programs for healthcare workers.
Optimal use of immunizing agents safeguards the health of
workers and protects patients from becoming infected through
exposure to infected workers.
The recommendations apply, but are not limited, to healthcare workers in acute-care hospitals; long-term–care facilities (e.g., nursing homes and skilled nursing facilities); physician’s offices; rehabilitation centers; urgent care centers, and outpatient clinics as well as to persons who provide home health care and emergency medical services (CDC, 2011a).
As per the recommendations of the Advisory Committee on Immunization Practices (ACIP) (CDC, 2011a), the following
Immunizations are recommended for healthcare personnel:
- Hepatitis B
- HCP and trainees in certain populations at high risk for chronic hepatitis B (e.g., those born in countries with high and intermediate endemicity) should be tested for HBsAg and anti-HBc/anti-HBs to determine infection status.
- Influenza
- Emphasis that all HCP, not just those with direct patient care duties, should receive an annual influenza vaccination
- Comprehensive programs to increase vaccine coverage among HCP are needed; influenza vaccination rates among HCP within facilities should be measured and reported regularly.
- Measles, mumps, and rubella (MMR)
- History of disease is no longer considered adequate presumptive evidence of measles or mumps immunity for HCP; laboratory confirmation of disease was added as acceptable presumptive evidence of immunity. History of disease has never been considered adequate evidence of immunity for rubella.
- The footnotes have been changed regarding the recommendations for personnel born before 1957 in routine and outbreak contexts. Specifically, guidance is provided for 2 doses of MMR for measles and mumps protection and 1 dose of MMR for rubella protection.
- Pertussis
- HCP, regardless of age, should receive a single dose of Tdap as soon as feasible if they have not previously received Tdap.
- The minimal interval was removed, and Tdap can now be administered regardless of interval since the last tetanus or diphtheria-containing vaccine.
- Hospitals and ambulatory-care facilities should provide Tdap for HCP and use approaches that maximize vaccination rates.
- Varicella
- Criteria for evidence of immunity to varicella were established. For HCP they include written documentation with 2 doses of vaccine,
- laboratory evidence of immunity or laboratory confirmation of disease,
- diagnosis of history of varicella disease by health-care provider, or diagnosis of history of herpes zoster by health-care provider.
- Meningococcal
- HCP with anatomic or functional asplenia or persistent complement component deficiencies should now receive a 2-dose series of meningococcal conjugate vaccine. HCP with HIV infection who are vaccinated should also receive a 2 dose series.
- Those HCP who remain in groups at high risk are recommended to be revaccinated every 5 years.
Abbreviations: HBsAg = Hepatitis B surface antigen; anti-HBc = hepatitis B core antibody; anti-HBs = hepatitis B surface antibody; Tdap = tetanus toxoid, reduced diptheria toxoid and acellular pertussis vaccine; HIV = human immunodeficiency virus. * Updated recommendations made since publication of the 1997 summary of recommendations (CDC Immunization of health-care workers: recommendations of the Advisory Committee on Immunization Practices [ACIP] and the Hospital Infection Control Practices Advisory Committee [HICPAC]. MMWR 1997;46[No. RR-18]).
In addition to pre-employment screening or testing for infection
and illness, vaccinations for vaccine-preventable illnesses,
maintenance of good health, and the utilization of engineering
and work practice controls are all methods to minimize the
risk of acquiring or transmitting an infectious disease.
During 1982, when hepatitis B vaccine was first recommended for healthcare personnel. an estimated 10,000 infections occurred among persons employed in a medical or dental field. By 2004, the number of HBV infections among HCP had decreased to an estimated 304 infections, largely resulting from the implementation of routine preexposure vaccination and improved infection-control precautions, such as Universal and Standard Precautions (CDC, 2011a).
Through December 2001, there were 57 documented cases of occupational HIV transmission to health care workers in the United States, and no confirmed cases have been reported since 1999 (CDC, 2011b).
Exposure prevention remains the primary strategy for reducing occupational bloodborne pathogen infections, CDC offers the following recommendations (CDC, 2011b), many of which have been covered more thoroughly in previous sections of this course.
Prevention Strategies
Health care workers should assume that the blood and other body fluids from all patients are potentially infectious. They should therefore follow infection control precautions at all times.
These precautions include:
- routinely using barriers (such as gloves and/ or goggles) when anticipating contact with blood or body fluids,
- immediately washing hands and other skin surfaces after contact with blood or body fluids, and
- carefully handling and disposing of sharp instruments during and after use.
Safety devices have been developed to help prevent needle-stick injuries. If used properly, these types of devices may reduce the risk of exposure to HIV. Many percutaneous injuries, such as needle-sticks and cuts, are related to sharps disposal. Strategies for safer disposal, including safer design of disposal containers and placement of containers, are being developed.
Building Better Prevention Programs for Health Care Workers
Continued diligence in the following areas is needed to help reduce the risk of occupational HIV transmission to health care workers.
Administrative efforts. All health care organizations should train health care workers in infection control procedures and on the importance of reporting occupational exposures. They should develop a system to monitor reporting and management of occupational exposures.
Development and promotion of safety devices. Effective and competitively priced devices engineered to prevent sharps injuries should continue to be developed for health care workers who frequently come into contact with potentially HIV-infected blood and other body fluids. Proper and consistent use of such safety devices should be continuously evaluated.
Monitoring the effects of PEP. Data on the safety and acceptability of different regimens of PEP, particularly those regimens that include new antiretroviral agents, should be continuously monitored and evaluated. Furthermore, improved communication about possible side effects before starting treatment and close follow-up of health care workers receiving treatment are needed to increase compliance with the PEP.
Although the most important strategy for reducing the risk of occupational HIV transmission is to prevent occupational exposures, plans for postexposure management of health care personnel should be in place. CDC has issued guidelines for the management of health care worker exposures to HIV and recommendations for postexposure prophylaxis (PEP): Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HIV and Recommendations for Postexposure Prophylaxis (September 30, 2005). These guidelines outline a number of considerations in determining whether health care workers should receive PEP and in choosing the type of PEP regimen. For most HIV exposures that warrant PEP, a basic 4-week, two-drug (there are several options) regimen is recommended. For HIV exposures that pose an increased risk of transmission (based on the infection status of the source and the type of exposure), a three-drug regimen may be recommended. Special circumstances, such as a delayed exposure report, unknown source person, pregnancy in the exposed person, resistance of the source virus to antiviral agents, and toxicity of PEP regimens, are also discussed in the guidelines. Occupational exposures should be considered urgent medical concerns (CDC, 2011b).
Exposure prevention remains the primary strategy for reducing
occupational bloodborne pathogen infections. However, occupational
exposures will continue to occur, and post exposure prophylaxis
(PEP) is an important element of exposure management (CDC,
2005).
Access to clinicians who can provide post-exposure care should
be available during all working hours, including nights and
weekends. Hepatitis B immunoglobulin (HBIG), HBV vaccine and
antiretroviral agents for post-exposure prophylaxis (PEP)
should be available in a timely manner, either by providing
access onsite or by developing linkages with providers or
facilities that can provide such service off-site. Those individuals
who are responsible to provide post-exposure management must
be knowledgeable about the evaluation and treatment protocols
and the facility's plans for accessing post-exposure medications
(CDC, 2005).
The recommendations provided by the CDC (See Tables 3 and
4) apply to situations in which healthcare providers have
been exposed to a source person who either has or is considered
likely to have HIV infection. These recommendations are based
on the risk for HIV infection after different types of exposure
and on limited data regarding efficacy and toxicity of PEP.
If PEP is offered and taken and the source is later determined
to be HIV-negative, PEP should be discontinued (CDC, 2005).
Although concerns have been expressed regarding HIV-negative
sources being in the window period for seroconversion, no
case of transmission involving an exposure source during the
window period has been reported in the United States. Rapid
HIV testing of source patients can facilitate making timely
decisions regarding use of HIV PEP after occupational exposures
to sources of unknown HIV status. Because the majority of
occupational HIV exposures do not result in transmission of
HIV, potential toxicity must be considered when prescribing
PEP. Because of the complexity of selecting HIV PEP regimens,
when possible, these recommendations should be implemented
in consultation with persons having expertise in antiretroviral
therapy and HIV transmission. Reevaluation of exposed healthcare
providers should be strongly encouraged within 72 hours postexposure,
especially as additional information about the exposure or
source person becomes available (CDC, 2005).
Healthcare workers must be informed to report occupational
exposures immediately after they occur because prophylactic
treatment is most effective when administered as soon after
the exposure as possible. PEP is preferably within hours rather
than days of exposure (CDC, 2005).
Healthcare facilities will have policies and procedures for
the prevention of occupational exposure in place as part of
their administrative controls related to infection control,
however, these facilities will also have policies and procedures
in place regarding reporting, evaluation, counseling, treatment
and follow-up of occupational exposure (CDC, 2005).
In the event that wounds or skin sites have been in contact
with blood or body fluids, the sites must immediately be washed
with soap and water; mucous membranes should be flushed with
water. No evidence exists that using antiseptics for wound
care or expressing fluid by squeezing the wound further reduces
the risk of transmission; however, the use of antiseptics
is not contraindicated (CDC, 2005).
In the event of an occupational exposure, the exposure and
post-exposure management should be recorded in the exposed
person's medical record. A facility may have a specific form
for such an exposure. Employers must follow all federal and
state requirements for recording and reporting occupational
injuries and exposures (CDC, 2005).
The CDC (2005) recommends that the following information
be recorded in the exposed person's confidential medical record:
- Date and time of exposure;
- Details of the procedure being performed, including where
and how the exposure occurred; if related to a sharp device,
the type and brand of device, and how and when in the course
of handling the device the exposure occurred;
- Details of the exposure, including type and amount of
fluid or material and the severity of the exposure (e.g.,
for a percutaneous exposure, depth of injury and whether
fluid was injected; for a skin or mucous membrane exposure,
the estimated volume of material) and the condition of the
skin (e.g., chapped abraded, intact).
- Details about the exposure source (e.g., whether the
source material contained HBV, HCV or HIV; if the source
is HIV-infected, the stage of disease, history of antiretroviral
therapy, viral load, antiretroviral resistance information,
if known).
- Details about the exposed person (e.g., HBV vaccination
and vaccine response status).
- Details about counseling, post-exposure management and
follow-up.
Basic and Expanded HIV Postexposure Prophylaxis Regimens
can be found in the Appendix of Updated US Public Health
Service Guidelines for the Management of Occupational Exposures
to HIV and Recommendations for Post Exposure Prophylaxis
(2005) available at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm
|
Table 1.
Recommended HIV postexposure prophylaxis (PEP) for percutaneous
injuries
|
|
Infection
Status of Source
|
|
Exposure
Type
|
HIV-Positive,
class 1*
|
HIV-positive,
class 2*
|
Source of
unknown HIV
status†
|
Unknown source§
|
HIV-negative
|
| Less severe¶ |
Recommend basic 2-drug PEP |
Recommend expanded >/= 3-drug PEP |
Generally, no PEP warranted; however, consider basic
2-drug PEP** for source with HIV risk factors†† |
Generally, no PEP warranted; however, consider basic
2-drug PEP** in settings in which exposure to HIV-infected
persons is likely |
No PEP warranted |
| More severe§§ |
Recommend expanded 3-drug PEP |
Recommend expanded >/= 3-drug PEP |
Generally, no PEP warranted; however, consider basic
2-drug PEP** for source with HIV risk factors†† |
Generally, no PEP warranted; however, consider basic
2-drug PEP** in settings in which exposure to HIV-infected
persons is likely |
No PEP warranted |
|
* HIV-positive, class 1 _ asymptomatic
HIV infection or known low viral load (e.g., <1,500
ribonucleic acid copies/mL). HIV-positive, class 2 -
symptomatic HIV infection, acquired immunodeficiency
syndrome, acute seroconversion, or known high viral
load. If drug resistance is a concern, obtain expert
consultation. Initiation of PEP should not be delayed
pending expert consultation, and, because expert consultations
alone cannot substitute for face-to-face counseling,
resources should be available to provide immediate evaluation
and follow-up care for all exposures.
† For example, deceased source person with no
samples available for HIV testing.
§
For example, a needle from a sharps disposal container.
¶ For example, solid needle or superficial injury.
** The recommendation "consider PEP" indicates
that PEP is optional; a decision to initiate PEP should
be based on discussion between the exposed person and
the treating clinician regarding the risks versus benefits
of PEP.
†† If PEP is offered and administered and
the source is later determined to be HIV-negative, PEP
should be discontinued.
§§
For example, large-bore hollow needle, deep puncture,
visible blood on device or needle used in patient's
artery or vein.
|
|
Table 2.
Recommended HIV postexposure prophylaxis (PEP) for mucous
membrane exposures and nonintact skin* exposures
|
|
Infection
status of source
|
|
Exposure
type
|
HIV-positive,
class 1†
|
HIV-positive
class 2†
|
Source of
unknown HIV
status§
|
Unknown
source¶
|
HIV-negative
|
| Small volume** |
Consider basic 2- drug PEP†† |
Recommend
2-drug PEP
|
Generally, no PEP warranted§§ |
Generally, no PEP warranted |
No PEP warranted |
| Large Volume¶¶ |
Recommend basic 2-drug PEP |
Recommend expanded >/= 3-drug PEP |
Generally, no PEP warranted; however, consider basic
2-drug PEP††
for source with HIV risk factors§§ |
Generally, no PEP warranted; consider basic 2-drug PEP††
in settings in which exposure to HIV-infected persons
is likely |
No PEP warranted |
|
* For skin exposures,
follow-up is indicated only if evidence exists of compromised
skin integrity (i.e., dermatitis, abrasion, or open
wound).
† HIV-positive, class 1 - asymptomatic HIV infection
or known low viral load (e.g., <1,500 ribonucleic
acid copies/ml). HIV-positive, class 2 - symptomatic
HIV infection, AIDS, acute seroconversion, or known
high viral load. If drug resistance is a concern, obtain
expert consultation. Initiation of PEP should not be
delayed pending expert consultation, and, because expert
consultation along cannot substitute for face-to-face
counseling, resources should be available to provide
immediate evaluation and follow-up care for all exposures.
§ For example, deceased source person with
no samples available for HIV testing.
¶ For example, splash from inappropriately disposed
blood.
**For example, a few drops.
§§ If PEP is offered and administered
and the source is later determined to be HIV-negative,
PEP should be discontinued.
¶¶ For example, a major blood splash.
|
Continue to
|
 |