 |
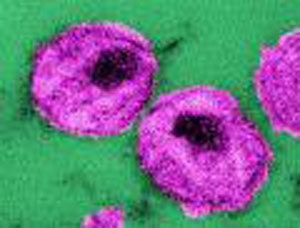 This thin-section transmission electron
micrograph (TEM) depicted the ultrastructural details of a
number of "human immunodeficiency virus" (HIV) virus
particles, or virions.
This thin-section transmission electron
micrograph (TEM) depicted the ultrastructural details of a
number of "human immunodeficiency virus" (HIV) virus
particles, or virions.
Photo courtesy of CDC; photo credit: Cynthia Goldsmith.
The National Healthcare Safety Network (NHSN) is a secure, internet-based surveillance system that integrates and expands legacy patient and healthcare personnel safety surveillance systems managed by the Division of Healthcare Quality Promotion (DHQP) at CDC. NHSN also includes a new component for hospitals to monitor adverse reactions and incidents associated with receipt of blood and blood products. Enrollment is open to all types of healthcare facilities in the United States, including acute care hospitals, long term acute care hospitals, psychiatric hospitals, rehabilitation hospitals, outpatient dialysis centers, ambulatory surgery centers, and long term care facilities. For more information, click on the topics below (CDC, 2013).
There are almost 2 million HAIs annually. Of those infections, 99,000 people die from these infections (USHHC, AHRQ, 2012). The following HAIs account for roughly two-thirds of all HAIs (CDC, 2012):
- Central line-associated bloodstream infections,
- Catheter-associated urinary tract infections,
- Ventilator-associated pneumonia. and
- Surgical site infections.
Additionally, Clostridium difficile can cause gastrointestinal infection; patients can be exposed to this bacterium through contaminated surfaces or the spores can be transferred on unclean hands of others. Central line-associated bloodstream infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia account for roughly two-thirds of all HAIs.
According to the CDC (2011), the following are pathogens and infectious diseases that can potentially be acquired in healthcare settings (these illnesses are linked to the CDC website in the event the learner would like more information about each disease):
In 2009, the CDC published the Direct Medical Costs of Healthcare-Associated Infections in US Hospitals and the Benefits of Prevention, (CDC and Scott, 2009). This report used results from published medical and economic literature to provide a range of estimates for the annual direct hospital cost of treating healthcare-associated infections (HAIs) in the United States. Applying two different Consumer Price Index (CPI) adjustments to account for the rate of inflation in hospital resource prices, the overall annual direct medical costs of HAI to U.S. hospitals ranges from $28.4 to $33.8 billion (after adjusting to 2007 dollars).
Clearly the prevalence of HAIs contributes significantly
to increased morbidity, mortality and cost in healthcare.
Therefore, it is critical that healthcare professionals do
all they can to minimize the risk that their behavior contributes
to the spread of infection.
Healthcare professionals, although well aware of the importance
of accepted principles and practices of infection control,
may at times, for multiple reasons, fail to follow these accepted
principles and practices. However, professionals have both
an ethical and professional responsibility to adhere
to scientifically accepted or evidence based practices and
principles of infection control.
There are multiple organizations that have developed "best practices" related to infection control. For example, the CDC has developed multiple guidelines for preventing infections in patients and healthcare personnel, as well as treatment guidelines, should exposure occur. These guidelines can be accessed from the CDC website http://www.cdc.gov/HAI/prevent/prevent_pubs.html.
Other organizations that focus on scientifically accepted
practices and principles of infection control include:
Multiple professional disciplines' Codes of Ethics
require that the professional maintain current knowledge in
the field.
In 1999 New York State included the legal responsibility
to adhere to such principles. A law was passed in which the
professional may be charged with unprofessional conduct if
he or she fails to adhere to scientifically accepted principles
and practices of infection control. This is true for the professional
her or himself, but also true for those whom the professional
has clinical or administrative oversight. In 2008, physicians,
physician assistants and specialist assistants were added
to the professions who had a legal responsibility to adhere
to scientifically accepted principles and practices of infection
control and they now can be disciplined if they fail to do
so.
Some examples of these legal requirements may include:
- An attending physician does not correct the resident physician
in the emergency room who has neglected to utilize the "sharps"
containers after giving injections to patients;
- A licensed practical nurse does not intervene to correct
a certified nursing assistant who does not wash his/her
hands after providing care to a resident in a long term
care facility;
- Certified nursing assistant, for whom the registered
nurse has supervisory responsibility, does not wash her
hands after removing gloves after completing care to a resident
in a long term care facility. The nurse can be charged with
unprofessional conduct if she does not intervene to correct
the situation;
- An registered nurse witnesses a colleague utilizing unsafe
injection practices and does nothing;
- A laboratory supervisor who looks the other way with one
lab technician, an excellent employee, who just can't seem
to remember to wear gloves during phlebotomy;
- A dentist who witnesses the assistant not changing gloves
between patients and does not intervene.
- A registered nurse, in the operating room, notes that
the temperature and the humidity in the storage room is
unusually high and wonders if the sterilized instruments
used by the OR staff may be contaminated, but takes no action.
All of the examples above illustrate that professionals must
take the responsibility to adhere to scientific principles
of infection control. They must themselves practice in such
a manner, but in addition, New York State Law requires that
these professionals must also insure that those for whom they
have administrative or clinical oversight also practice to
this standard. Professionals who fail to follow accepted standards
of infection control will have the complaint investigated.
Possible outcomes of such charges include: disciplinary action,
revocation of professional license and professional liability.
Continue to
|
 |