|
Hand Hygiene
The most common way that infection is spread throughout the
healthcare system is through hand contact. Indeed, handwashing
and hand hygiene are the single most effects means of limiting
the spread of infection. Despite the sophistication of healthcare
and the science behind that care, the simple and low-tech
intervention of hand hygiene is a significant factor in reducing
the spread of infection.
Handwashing should occur (CDC, 2002):
- Whenever hands are visibly dirty or contaminated.
- Before:
- having contact with patients
- putting on gloves
- inserting any invasive device
- manipulating an invasive device
- After:
- having contact with a patient's skin
- having contact with bodily fluids or excretions,
non-intact skin, wound dressings, contaminated items
- having contact with inanimate objects near a patient
- removing gloves
Alcohol-bashed hand rubs, either foam or gel, kill more effectively
and more quickly than handwashing with soap and water. They
are also less damaging to the skin, resulting in less dryness
and irritation, leading to fewer breaks in the skin. Hand
rubs require less time than handwashing with soap and water
and bottles/dispensers can be conveniently placed at the point
of care, to be more accessible (CDC, 2002).
ALCOHOL-BASED HAND
RUBS ARE MORE EFFECTIVE IN KILLING BACTERIA THAN SOAP AND
WATER
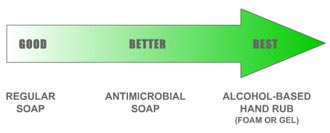
An alcohol-based hand rub is the preferred method
for hand hygiene in all situations, except for when your hands
are visibly dirty or contaminated.
HAND RUB (foam and gel)
- Apply to palm of one hand (the amount used depends on
specific hand rub product).
- Rub hands together, covering all surfaces, focusing in
particular on the fingertips and fingernails, until dry.
Use enough rub to require at least 15 seconds to dry.
HANDWASHING
- Wet hands with water.
- Apply soap.
- Rub hands together for at least 15 seconds, covering
all surfaces, focusing on fingertips and fingernails.
- Rinse under running water and dry with disposable towel.
- Use the towel to turn off the faucet.
Sharp instruments and disposable items must be properly
handled and disposed. Needles are NOT to be recapped,
purposely bent or broken, removed from disposable syringes
or otherwise manipulated by hand. After they are used, disposable
syringes and needles, scalpel blades and other sharp items
are to be placed in puncture-resistant, labeled containers
for sharps disposal. It is important that these containers
be conveniently located, as close as possible to where they
will be used. Additionally, it is important to not overfill
the sharps containers as placing items into these containers
poses risk when the container is overflowing with needles,
syringes and other sharp objects.
Housekeeping is important to maintain the work area
in a clean and sanitary condition. The employer is required
to determine and implement a written schedule for cleaning
and disinfection based on the location within the facility,
type of surface to be cleaned, type of soil present and tasks
or procedures being performed. All equipment, environmental
and working surfaces must be properly cleaned and disinfected
after contact with blood or OPIM.
Potentially contaminated broken glassware must be
removed using mechanical means, like a brush and dustpan or
vacuum cleaner. Specimens of blood or OPIM must be placed
in a closeable, labeled or color-coded leakproof container
prior to being stored or transported.
Chemical germicides and disinfectants used at recommended
dilutions must be used to decontaminate spills of blood and
other body fluids. Consult the Environmental Protection Agency
(EPA) lists of registered sterilants, tuberculocidal disinfectants,
and antimicrobials with HIV efficacy claims for verification
that the disinfectant used is appropriate. The lists are available
from the National Antimicrobial Information Network at (800)
858-7378 or http://npic.orst.edu/ptype/amicrob/pathogens.html.
Laundry that is or may be soiled with blood or OPIM,
and/or may contain contaminated sharps, must be treated as
though contaminated. Contaminated laundry must be bagged at
the location where it was used, and shall not be sorted or
rinsed in patient-care areas. It must be placed and transported
in bags that are labeled or color-coded (red-bagged).
Laundry workers must wear protective gloves and other appropriate
personal protective clothing when handling potentially contaminated
laundry. All contaminated laundry must be cleaned or laundered
so that any infectious agents are destroyed.
Waste disposal procedures must be carefully followed.
All infectious waste must be placed in closeable, leakproof
containers or bags that are color-coded (red-bagged) or labeled
as required to prevent leakage during handling, storage and
transport. Disposal of waste shall be in accordance with federal,
state and local regulations.
Tags or labels must be used as a means to prevent
accidental injury or illness to employees who are exposed
to hazardous or potentially hazardous conditions, equipment
or operations which are out of the ordinary, unexpected or
not readily apparent. Tags must be used until the identified
hazard is eliminated or the hazardous operation is completed.
Personal activities such as eating, drinking,
smoking, applying cosmetics or lip balm, and handling contact
lenses are prohibited in laboratories and other work areas
where blood or OPIM are present.
Food and drink must not be stored in refrigerators,
freezers or cabinets where blood or OPIM are stored, or in
other areas of possible contamination.
Bloodborne Pathogen Training
All new employees or employees being transferred into jobs
involving tasks or activities with potential exposure to blood/OPIM
shall receive training in the Bloodborne Pathogen Standard
at the time of initial assignment to the tasks where occupational
exposure may occur. This training will include information
on the hazards associated with blood/OPIM, the protective
measures to be taken to minimize the risk of occupational
exposure, and information on the appropriate actions to take
if an exposure occurs.
Retraining is required annually, or when changes in procedures
or tasks affecting occupational exposure occur. As previously
mentioned, the limited information in this section does not
qualify for the full training.
All employees whose jobs involve participation in tasks or
activities with exposure to blood/OPIM shall be offered the
start of the Hepatitis B vaccination series within
10 working days of employment and/or new assignment. The vaccine
will be provided free of charge. Serologic testing after vaccination
(to ensure that the shots were effective) is recommended for
all persons with occupational exposures.
Risk of Occupational exposures
The CDC states that the risk of infection for HIV, HBV or
HCV in the healthcare setting varies from case by case. Factors
influencing the risk of infection from occupational exposure
are:
- Whether the exposure was from a hollow-bore needle or
other sharp instrument;
- To intact skin or mucus membranes (such as the eyes,
nose, mouth);
- The amount of blood that was involved and
- The amount of virus present in the source's blood
The risk of HIV infection to a healthcare worker through
a needlestick is less than 1%. Approximately 1 in 300 exposures
through a needle or sharp instrument result in infection.
The risks of HIV infection through splashes of blood to the
eyes, nose or mouth is even smaller - approximately 1 in 1,000.
There have been no reports of HIV transmission from blood
contact with intact skin. There is a theoretical risk of blood
contact to an area of skin that is damaged, or from a large
area of skin covered in blood for a long period of time. In
2001, the CDC reported 56 documented cases and 138 possible
cases of occupational exposure to HIV since reporting started
in 1985. The risk of getting HBV from a needlestick or cut
is between 6-30%, unless the person exposed has been vaccinated
to hepatitis B. There are only a few studies regarding the
risk of getting HCV from occupational exposure. The risk of
getting HCV from a needlestick or cut is between 2-3%. The
risk of getting HBV or HCV from a blood splash to the eyes,
nose or mouth is possible but believed to be very small. As
of 1999, about 800 health care workers a year are reported
to be infected with HBV following occupational exposure. There
are no exact estimates on how many healthcare workers contract
HCV from an occupational exposure. To put this in perspective,
the risk of a healthcare worker contracting HCV from an accidental
needlestick is 20-40% greater than their risk of contracting
HIV.
Treatment After a Potential Occupational
Exposure
It is important to follow the protocol of your employer.
The CDC recommends that post-exposure prophylaxis should be
started ideally within 2 hours of occupational exposure (CDC,2005).
The CDC recommends that as soon as safely possible, wash the
affected area(s). Application of antiseptics should not be
a substitute for washing. It is recommended that any potentially
contaminated clothing be removed as soon as possible. It is
also recommended that you familiarize yourself with existing
protocols and the location of emergency eyewash or showers
and other stations within your facility.
If the HIV exposure is to the eyes, nose or mouth, flush
them continuously with water, saline or sterile irrigants
for at least five minutes. The risk of contracting HIV through
this type of exposure is estimated to be 0.09%.
In the event of a needlestick injury, wash the exposed area
with soap and clean water. Do not "milk" or squeeze the wound.
There is no evidence that shows using antiseptics (like hydrogen
peroxide) will reduce the risk of transmission for any bloodborne
pathogens. In the event that the wound needs suturing, emergency
treatment should be obtained. The risk of contracting HIV
from this type of exposure is estimated to be 0.3%.
Exposure to saliva is not considered substantial unless
there is visible contamination with blood. Wash the area with
soap and water, and cover with a sterile dressing as appropriate.
All bites should be evaluated by a healthcare professional.
Exposure to urine, feces, vomit or sputum is not considered
substantial unless the fluid is visibly contaminated with
blood. Follow normal procedures for cleaning these fluids.
Reporting the Exposure
Follow the protocol of your employer. The following general
guidelines taken from the CDC are not meant to replace an
existing protocol. After cleaning the exposed area as recommended
above, report the exposure to the department or individual
at your workplace that is responsible for managing exposure.
Obtain medical evaluation as soon as possible. Discuss with
a healthcare professional the extent of the exposure, prophylaxis/prevention
of other bloodborne pathogens, the need for a tetanus shot
and other care.
Post-exposure Prophylaxis
Post-exposure prophylaxis (PEP) provides anti-HIV medications
to someone who has had a substantial exposure, usually to
blood. PEP has been the standard of care for occupationally-exposed
healthcare workers with substantial exposures since 1996.
Animal models suggest that cellular HIV infection happens
within 2 days of exposure to HIV. Virus in blood is detectable
within 5 days. Therefore, PEP should be started as soon as
possible, optimally within 2 hours, preferably within 24
hours of the exposure or as soon as possible and continued
for 28 days. However, PEP for HIV does not provide prevention
of other bloodborne diseases, like HBV or HCV.
HBV PEP for susceptible persons would include administration
of hepatitis B immune globulin and HBV vaccine. This should
occur as soon as possible and no later than 7 days post-exposure.
There are currently no recommendations for HCV exposure.
There have been several changes in CDC (2005) recommendations
for post-exposure prophylaxis (PEP). These changes are based
on new scientific evidence that resulted from research focused
on viral transmission following occupational and non-occupational
exposures. The most current recommendations can be found at
the CDC website and are available in downloadable format for
use in emergency departments and medical offices.
The CDC (2005) currently recommends PEP for occupational
exposures:
PEP should be initiated as soon as possible, preferably
within hours rather than days of exposure. If a question
exists concerning which antiretroviral drugs to use, or
whether to use a basic or expanded regimen, the basic regimen
should be started immediately rather than delay PEP administration.
The optimal duration of PEP is unknown. Because 4 weeks
of zidovudine appeared protective in occupational and animal
studies, PEP should be administered for 4 weeks, if tolerated.
Combinations that can be considered for PEP include ZDV
and 3TC or emtricitabine (FTC); d4T and 3TC or FTC; and
tenofovir (TDF) and 3TC or FTC. In the previous Public Health
Service guidelines, a combination of d4T and ddI was considered
one of the first-choice PEP regimens; however, this regimen
is no longer recommended because of concerns about toxicity
(especially neuropathy and pancreatitis) and the availability
of more tolerable alternative regimens.
The PI preferred for use in expanded PEP regimens is lopinavir/ritonavir
(LPV/RTV). Other PIs acceptable for use in expanded PEP
regimens include atazanavir, fosamprenavir, ritonavir-boosted
indinavir, ritonavir-boosted saquinavir, or nelfinavir.
Although side effects are common with Non-nucleoside Reverse
Transcriptase inhibitors, efavirenz may be considered for
expanded PEP regimens, especially when resistance to PIs
in the source person's virus is known or suspected. Caution
is advised when EFV is used in women of childbearing age
because of the risk of teratogenicity (CDC, 2005).
For non-occupational exposures (nPEP), the recommendations
are as follows:
For persons seeking care <72 hours after non-occupational
exposure to blood, genital secretions, or other potentially
infectious body fluids of a person known to be HIV infected,
when that exposure represents a substantial risk for transmission,
a 28-day course of highly active antiretroviral therapy
(HAART) is recommended. Antiretroviral medications should
be initiated as soon as possible after exposure. For persons
seeking care <72 hours after non-occupational exposure to
blood, genital secretions, or other potentially infectious
body fluids of a person of unknown HIV status, when such
exposure would represent a substantial risk for transmission
if the source were HIV infected, no recommendations are
made for the use of nPEP. Clinicians should evaluate risks
and benefits of nPEP on a case-by-case basis. For persons
with exposure histories that represent no substantial risk
for HIV transmission or who seek care >72 hours after exposure,
DHHS does not recommend the use of nPEP (CDC, 2005a).
Post-exposure prophylaxis can only be obtained from a licensed
healthcare provider. Your facility may have recommendations
and a chain of command in place for you to obtain PEP. After
evaluation of the exposure route and other risk factors, certain
anti-HIV medications may be prescribed.
The specific details about post-exposure management and treatment
see the CDC (2005) Updated US Public Health Guidelines for
the management of occupational exposures to HIV and recommendations
for postexposure prophylaxis. MMWR, 54(RR09), 1-17, available
at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm.
PEP is not as simple as swallowing one pill. The medications
must be started within the first 2 hours if possible, and
continued for 28 days. Many people experience significant
medication side effects.
It is very important to report occupational exposure to
the department at your workplace that is responsible for managing
exposure. If post-exposure treatment is recommended, it should
be started as soon as possible.
In rural areas, police, firefighters and other at-risk emergency
providers should identify a 24-hour source for PEP. The national
bloodborne pathogen hotline provides 24-hour consultation
for clinicians who have been exposed on the job. Call 1-888-448-4911
for the latest information on prophylaxis for HIV, hepatitis,
and other pathogens.
HIV/HBV/HCV Testing Post-exposure
As a healthcare professional, if one sustains an occupational
exposure to HIV, HBV and HCV, antibody testing for HIV, HBV
and HCV, as well as vaccination for HBV will be offered. Since
it usually takes the body between two weeks and three months
to produce antibodies to HIV, the initial test serves as a
baseline. It will show whether HIV infection occurred prior
to this exposure. Additional testing will be needed. In 2001,
the CDC recommended retesting at six weeks, 3 and 6 months
after exposure. Testing for up to 12 months may be recommended
for high risk exposures or when the source is documented to
be infected with HIV. The need for a Hepatitis B titer test
(if previously vaccinated for HBV), tests for elevated liver
enzymes and other available testing for other bloodborne pathogens
should be discussed with the healthcare provider.
There are situations where healthcare workers and others
are not aware of the HIV status of the individual to whose
blood they have been exposed. Usually, you can't force someone
to test for HIV and reveal their results to you.
If an occupational exposure occurs, the exposed person can
request HIV testing of the source individual. However, the
source must consent to the testing. Source testing does not
eliminate the need for baseline testing of the exposed individual
for HIV, HBV, HCV and liver enzymes. Provision of PEP should
also not be contingent upon the results of a source's test.
Current wisdom indicates immediate provision of PEP, with
discontinuation of treatment based upon the source's test
results.
The risk of HIV infection to a healthcare worker from a needlestick
containing HIV-positive blood is about 1 in 300, according
to CDC data. Risks for infection with found syringes will
depend on a variety of factors, including the amount of time
the syringe was left out, presence of blood and the type of
injury (scratch versus puncture).
Continue on to Legal
Aspects of HIV/AIDS: Testing, Counseling and Confidentiality
|