|
People of Color
African Americans and Hispanics specifically
have disproportionately higher rates of AIDS cases in the
U.S., despite the fact that there are no biological reasons
for the disparities.
Figure 2. below illustrates the distribution
of AIDS cases reported in 2003 among racial/ethnic groups.
The pie chart on the right shows the distribution of the US
population (excluding US dependencies, possessions and associated
nations) in 2003.
Non-Hispanic blacks and Hispanics are disproportionately
affected by the AIDS epidemic in comparison with their proportional
distribution in the general population. In 2003, non-Hispanic
blacks made up 13% of the population but accounted for 48%
of reported AIDS cases. Hispanics made up 14% of the population
but accounted for 18% of reported AIDS cases.
Non-Hispanic whites made up 69% of the US population
but accounted for 31% of reported AIDS cases.
Figure 2. Proportion of Reported AIDS Cases
and Population, by Race/Ethnicity, 2003-50 States and D.C.
(CDC, 2005b). 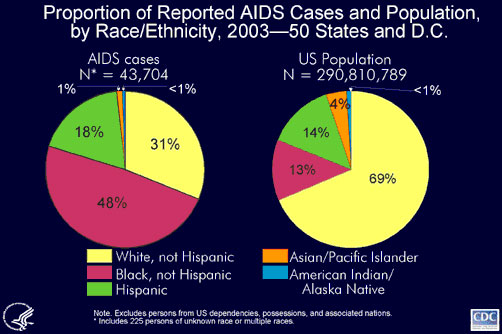
There is not one single reason that stands out
as to why the disparities exist. Multiple factors contribute
to racial/ethnic health disparities, including socioeconomic
factors (e.g., education, employment, and income), lifestyle
behaviors (e.g., physical activity and alcohol intake), social
environment (e.g., educational and economic opportunities,
racial/ethnic discrimination, and neighborhood and work conditions),
and access to preventive health-care services (e.g., cancer
screening and vaccination) (CDC, 2005c). Both legacies of
the past and current issues of race mean that many people
of Color do not trust "the system" for a variety of reasons.
Thus, even when income is not a barrier, access to early intervention
and treatment may be limited. And HIV may be only one of a
list of problems, which also include adequate housing, food,
employment, etc.

Photograph by Lloyd Wolf for the U.S. Census
Bureau, Public Information Office
Recent immigrants also can be at increased risk
for chronic disease and injury, particularly those who lack
fluency in English and familiarity with the U.S. healthcare
system or who have different cultural attitudes about the
use of traditional versus conventional medicine. Approximately
6% of persons who identified themselves as Black or African
American in the 2000 census were foreign-born (CDC, 2005c).

Photo by the U.S. Census Bureau, Public Information
Office
For African Americans in the US, health disparities
can mean earlier deaths, decreased quality of life, loss of
economic opportunities, and perceptions of injustice. For
society, these disparities translate into less than optimal
productivity, higher health-care costs, and social inequity.
By 2050, an estimated 61 million African American persons
will reside in the US, amounting to approximately 15% of the
total US population (CDC, 2005c).
Another factor may be the diversities within
these populations. Diversity is evident in immigrant status,
religion, languages, geographic locations and, again, socioeconomic
conditions. Getting information out in appropriate ways to
these diverse populations has been difficult.
There is a significant amount of denial about
HIV risk, which continues to exist in these communities. As
with other groups, there may also be fear and stigmatization
of those who have HIV. Prevention messages need to be tailored
in ways that are culturally appropriate and relevant. The
messages must be carried through channels that are appropriate
for the individual community. These channels may include religious
institutions or through respected "elders" in the community.
Ironically, it may be these institutions or elders who, in
the past, have contributed to the misinformation and stigma
associated with HIV. Many HIV prevention programs are recognizing
the need to work within these diverse communities to let the
communities lead the way in prevention the transmission of
HIV.
Adolescents/Young Adults
The effects of HIV and AIDS among adolescents
and young adults (ages 13 to 24) in the United States continues
to be an increasing concern. The CDC reported 38,490 cumulative
cases of AIDS among people ages 13 to 24 through 2003. Since
the epidemic began, an estimated 10,041 adolescents and young
adults with AIDS have died and the proportion diagnosed with
AIDS is increasing. Also, the proportion with an AIDS diagnosis
among adolescents and young adults has increased from 3.9
percent in 1999 to 4.7 percent in 2003 (NIAID, 2005).
Moreover, African-American and Hispanic adolescents
have been disproportionately affected by the HIV/AIDS epidemic.
Between the ages of 13 and 19, African-Americans and Hispanics
accounted for 66 percent and 21 percent, respectively, of
the reported AIDS cases in 2003 (NIAID, 2005).
Because the average duration from HIV infection
to the development of AIDS is 10 years, most adults with AIDS
were likely infected as adolescents or young adults. In 2003,
an estimated 3,897 were diagnosed with HIV/AIDS, while an
estimated 13,752 were living with HIV/AIDS. Health experts
estimate the number of adolescents and adults living with
HIV infection, however, to be much higher (NIAID, 2005).
Most HIV-infected adolescents and young adults
are exposed to the virus through sexual intercourse. Recent
HIV surveillance data suggest that the majority of HIV-infected
adolescent and young adult males are infected through sex
with men. Only a small percentage of males appear to be exposed
by injection drug use and/or heterosexual contact. The same
data also suggest that adolescent and young adult females
infected with HIV were exposed through heterosexual contact,
with a very small percentage through injection drug use. In
addition, there is an increasing number of children who were
infected as infants that are now surviving to adolescence
(NIAID, 2005).
Table 1. AIDS Cases among Male Adolescents
and Young Adults by Transmission Category, Cumulative through
2003-United States (CDC, 2005d). 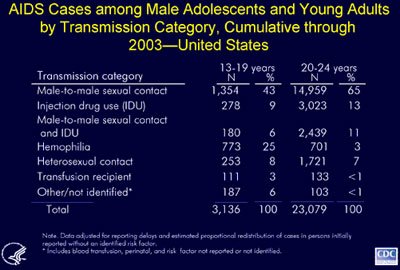
Nationally, since the beginning of the epidemic,
more than 3,100 adolescent males aged 13 to 19 years and approximately
23,000 young adult males aged 20 to 24 years have been reported
with AIDS (CDC, 2005d).
The majority (65%) of males aged 20 to 24 with
AIDS had a risk factor of male-to-male sexual contact and
an additional 11% were among males who reported risk factors
of male-to-male sexual contact and injection drug use (CDC,
2005d).
Approximately 25% of AIDS cases among adolescent
males aged 13-19 were among those who had hemophilia and acquired
their infection before blood products were heat treated to
prevent HIV transmission. In contrast, 3% of AIDS cases among
males aged 20-24 were attributed to receipt of blood products
for hemophilia (CDC, 2005d).
Injection drug use is more common among the
20 to 24 year old males reported with AIDS than among adolescents
with AIDS, but less common than among males over 24 years.
Eight percent of AIDS cases among males aged 13 to 19 and
7% of cases among males aged 20-24 years were reported with
heterosexual contact as their transmission category (CDC,
2005d).
Table 2. AIDS Cases among Female Adolescents
and Young Adults, by Transmission Category Cumulative through
2003-United States (CDC, 2005d).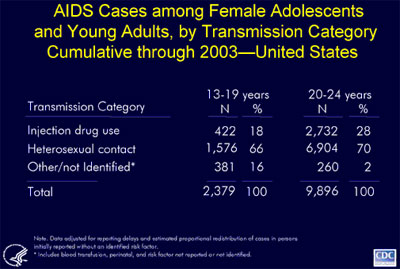
Approximately two-thirds of AIDS cases among
adolescent and young adult females were attributed to heterosexual
contact as the mode of exposure to HIV. Cases among adolescent
females were less likely to be attributed to injection drug
use than were cases among young adults (18% vs. 28% of cases)
(CDC, 2005d).

Photograph by Lloyd Wolf for the U.S. Census
Bureau, Public Information Office
Photograph by Heather Schmaedeke for U.S. Census
Bureau, Public Information Office
Approximately 25 percent of cases of sexually
transmitted infections (STIs) reported in the United States
each year are among teenagers. This is particularly significant
because the risk of HIV transmission increases substantially
if either partner is infected with an STI. Discharge of pus
and mucus as a result of STIs such as gonorrhea or chlamydia
infection also increase the risk of HIV transmission three-
to five-fold. Likewise, STI-induced ulcers from syphilis or
genital herpes increase the risk of HIV transmission nine-fold
(NIAID, 2005).
Adolescents and young adults tend to think they
are invincible and, therefore, deny any risks. This belief
may cause them to engage in risky behavior, delay HIV testing,
and if they test positive, delay or refuse treatment. The
inability to link them to medical care can lead to increased
transmission of HIV. Healthcare providers report that many
young people, when they learn they are HIV-positive, take
several months to accept their diagnosis and return for treatment
(NIAID, 2005).
Healthcare providers may be able to help young
people understand their situation during visits by (NIAID,
2005):
- Ensuring confidentiality.
- Explaining the information clearly.
- Eliciting questions.
- Emphasizing the success of newly available treatments.
The U.S. Department of Health and Human Services (DHHS) has
developed documents that address the standard of care for
the treatment of HIV, including information about how to treat
HIV in adolescents. The documents Guidelines for the Use
of Antiretroviral Agents in HIV-Infected Adults and Adolescents
and Guidelines for the Use of Antiretroviral Agents in Pediatric
HIV Infection are available from AIDSinfo.
According to the Guidelines for the Use of Antiretroviral
Agents in HIV-Infected Adults and Adolescents, adolescents
exposed to HIV sexually or via injection drug use appear to
follow a clinical course that is more similar to HIV disease
in adults than in children. Most adolescents with sexually
acquired HIV are in a relatively early stage of infection
and are ideal candidates for early intervention that includes
education and counseling, identifying high-risk behaviors,
and recommended therapies and behavioral changes (NIAID, 2005).
Adolescents who were infected at birth or via blood products
as young children, however, follow a unique clinical course
that may differ from that of other adolescents and adults.
Healthcare providers should refer to the treatment guidelines
for detailed information about treating HIV-infected adolescents
(NIAID, 2005).
Children
Children show significant differences in their HIV disease
progression and their virologic and immunologic responses,
compared to adults. Without drug treatment, children may have
developmental delay, pneumocystis carinii pneumonia, failure
to thrive, recurrent bacterial infections and other conditions
related to HIV.

Photograph by Lloyd Wolf for the U.S. Census
Bureau, Public Information Office
The antiretroviral treatments that are available
for HIV infection may not be available in pediatric formulations.
The medications may have different side effects in children
than they do in adults.

It is vital that women know their HIV status
before or during pregnancy. Antiretroviral treatment significantly
reduces the chance that their child will become infected with
HIV. Prior to the development of antiretroviral therapies,
most HIV-infected children were very sick by seven years of
age. In 1994, scientists discovered that a short treatment
course of the medication AZT for pregnant women dramatically
reduced the number, and rate, of children who became infected
perinatally. C-sections for delivery in certain cases may
be warranted to reduce HIV transmission. As a result, perinatal
HIV infections have substantially declined in the developed
world.
Early diagnosis of HIV infection in newborns
is now possible. Antiretroviral therapy for infants is now
the standard of care, and should be started as soon as the
child is determined by testing to be HIV-infected. Current
recommendations are to treat apparently uninfected children
who are born to mothers who are HIV-positive with antiretroviral
medicines for six weeks, to reduce any possibility of HIV
transmission.
Persons Aged 50 and
Older
A growing number of older people now have HIV/AIDS.
About 19 percent of all people with HIV/AIDS in this country
are age 50 and older. Numbers of cases are expected to increase,
as people of all ages survive longer due to triple-combination
drug therapy and other treatment advances (NIA, 2005; NAHOF,
nd).
|
|
|
|
|
Courtesy of Administration
on Aging
|
But there may even be many more cases than we
know about. Why? One reason may be that healthcare providers
do not always test older people for HIV/AIDS and so may miss
some cases during routine check-ups. Another may be that older
people often mistake signs of HIV/AIDS for the aches and pains
of normal aging, so they are less likely than younger people
to get tested for the disease. Also, they may be ashamed or
afraid of being tested. People age 50 and older may have the
virus for years before being tested. By the time they are
diagnosed with HIV/AIDS, the virus may be in the late stages
(NIA, 2005).
Older people with HIV/AIDS face a double stigma:
ageism and infection with a sexually-or-IV-drug transmitted
disease (NAHOF, nd). The number of HIV/AIDS cases among older
people is growing every year because (NIA, 2005):
- Older Americans know less about HIV/AIDS than younger
people.
- They do not always know how it spreads or the importance
of using condoms, not sharing needles, getting tested for
HIV, and talking about it with their doctor or other healthcare
provider.
- Healthcare workers and educators often do not talk with
middle-age and older people about HIV/AIDS prevention.
- Older people are less likely than younger people to talk
about their sex lives or drug use with their doctors or
other healthcare providers.
- Doctors and other healthcare providers may not ask older
patients about their sex lives or drug use, or talk to them
about risky behaviors.
The number of cases of HIV/AIDS for older women
has particularly been growing over the past few years. The
rise in the number of cases in women of color age 50 and older
has been especially steep. Most got the virus from sex with
infected partners. Many others got HIV through shared needles
(NIA, 2005).
Because women may live longer than men, and
because of the high divorce rate, many widowed, divorced,
and separated women are dating these days. Like older men,
many older women may be at risk because they do not know how
HIV/AIDS is spread. Women who no longer worry about getting
pregnant may be less likely to use a condom and to practice
safe sex. Also, vaginal dryness and thinning often occurs
as women age; when that happens, sexual activity can lead
to small cuts and tears that raise the risk for HIV/AIDS (NIA,
2005).
Advice for Victims
of Sexual Assault
There are likely to be between 172,400 - 683,000
females raped each year in the U.S. Men can also be victims
of sexual assault, but data and reporting are limited. Based
on existing crime report data, an estimated 40% of female
rape victims are under age 18; most sexual assault victims
know their assailant. Apart from the emotional and physical
trauma that accompanies sexual assault, there are other considerations.
Many victims do not report their attack to the police.
According to CDC, the odds of HIV infection
from a sexual assault in the U.S. are 2 in 1,000. There are
additional risks for contracting other STDs, and females can
become pregnant. Emergency contraception is part of the medical
treatment for female rape victims. The emergency contraception
hotline number, 1-888-668-2528, should be provided by telephone
rape counselors or other counselors.
Most experts recommend that a sexual assault
victim go directly to the nearest hospital emergency room,
without changing their clothing, bathing or showering first.
Trained staff in the emergency room will counsel the victim,
and may also offer testing or referral for HIV, STDs and pregnancy.
It is common practice for the emergency room physician to
take DNA samples of blood or semen from the vagina, rectum,
etc. which can be used as evidence against the attacker. Some
emergency departments may refer sexual assault survivors to
the local health jurisdiction for HIV testing.
Many people feel that the emergency room setting
is a profoundly unpleasant time to question a sexual assault
victim regarding her/his sexual risks, etc. However, testing
shortly after a sexual assault will provide baseline information
on her/his status for the various infections. This information
can be useful for the victim and healthcare provider, especially
for follow-up care and treatment. Additionally, baseline information
can be used for legal and criminal action against the assailant.
Continue on to Management
of HIV in the Healthcare Workplace
|